Be watchful over your health. A truly wealthy person, is a healthy person. High BP is a silent killer and a trigger to many health issues.

Clement C. Aladi. Department of Electrical Engineering. Biomedical Engineering
Seaver college of science and Engineering, Loyola Marymount University Los Angeles, California USA
Abstract— High blood pressure (hypertension) has been a life-threatening disease that has cost the lives of many, mainly among the black race in developing countries like Nigeria. The exact cause of hypertension is not known but many factors contribute to it, hence it can be controlled but not cured. Many in this condition are unaware of it and therefore it poses a greater health risk to their survival. The best protection, therefore, is knowledge, management, and prevention.
The health care system in Nigeria urgently needs to be improved with new technologies. Mobile health will go a long way to helping hypertensive people in the country. In this project, developing a mobile wearable device (like a normal wrist watch) that can monitor the blood pressure and gives a signal when it is high and life-threatening will be surveyed. This wearable device will function in a way different from what is already in the US market and taking into consideration the unavailability of a 911 emergency system and the poor health care system in Nigeria.
I. INTRODUCTION
I am a Nigerian brought up in the Eastern part of the country. As a child I heard of many who died of high blood pressure{hypertension} and as an adult I have continue to experience the same. Due to inaccessibility and high cost of health care many with this health condition don’t know they have it. According to WHO 40% of the world’s population is hypertensive. Nigeria has a population of 170 million with 50% of this number hypertensive.
Most people with high blood pressure have no signs or symptoms, even if blood pressure readings reach dangerously high levels.
A few people with high blood pressure may have headaches, shortness of breath or nosebleeds, but these signs and symptoms aren’t specific and usually don’t occur until high blood pressure has reached a severe life-threatening stage.
This work aims at developing a wearable blood pressure monitoring system to help hypertensive people manage their BP. This device, which has the size and look of a wristwatch, can monitor pressure continuously—which provides a much more accurate picture than infrequent readings in the doctor’s office. Until now, the only way to do such continuous monitoring has been with a cumbersome inflatable cuff for the arm or wrist.






II. WHAT IS BLOOD PRESSURE?
Blood pressure is the force/pressure of the blood pushing against the walls of the arteries. With each heartbeat, blood is being pumped out into our arteries and throughout the body.
III. WHAT IS HYPERTENSION?
Hypertension, or high blood pressure, is classified as a blood pressure measurement of 140/90 mmHg or above. According to the American Heart Association, hypertension affects nearly one out of every three Americans. Hypertension is a major risk factor associated with many cardiovascular diseases and plays a significant role in the progression of congestive heart failure, stroke, heart attacks, kidney failure, and premature death. Factors that contribute to the prevalence of hypertension are smoking, stress, drugs, alcohol, nutrition, diabetes, obesity, and limited physical activity.
IV. WHY WEARABLE A BLOOD PRESSURE MONITOR?
We are considering a wearable device because the driving force of the technological development is moving tests from lab or Hospital to home, from point of care (POC) to remote or even mobile, from professional to self-care, from inconvenient to convenient and from expensive to cheap
Secondly there is need for wearable fitness device that could monitor your blood pressure continuously, 24 hours a day since existing devices don’t have that capability; blood pressure (BP) measurements currently in use require the use of a cuff that temporarily stops blood flow.
V. WHAT ARE THE RISKS AND THE CONSEQUENCES OF HIGH BP
The following could pre-dispose one to high blood pressure:
Age, Race, family history, being overweight or obese, not being physically active, using tobacco/ drinking too much alcohol, too much salt in diet/too little potassium in diet, stress, certain chronic conditions. Hypertension could lead loss of vision, stroke, Heart failure, Heart attack, sexual dysfunction and Kidney disease/ failure
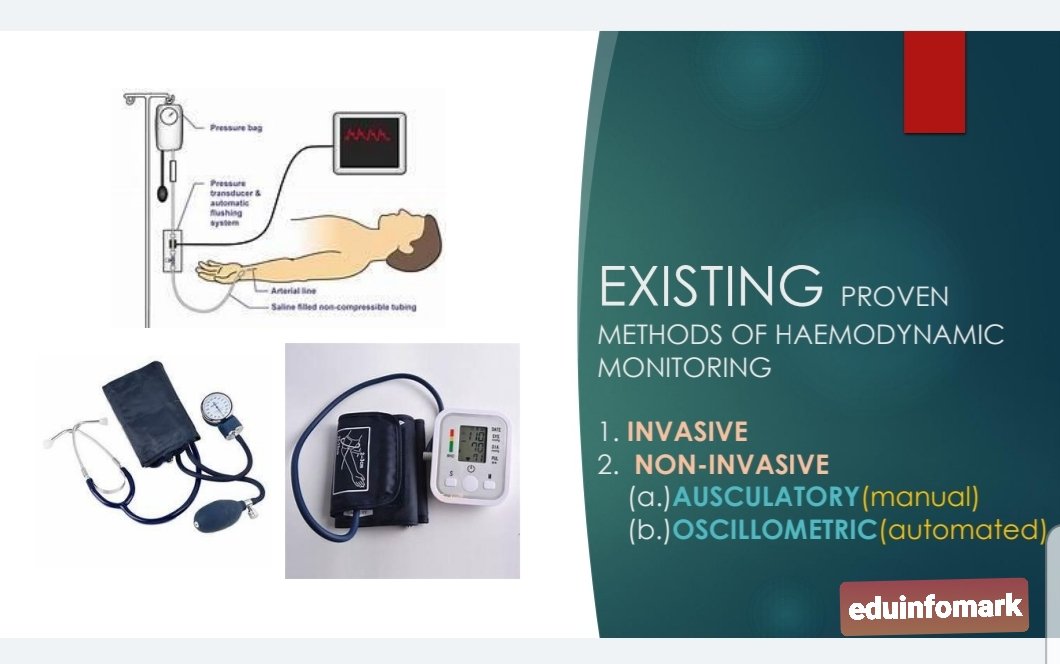
VI. EXISTING METHODS OFHAEMODYNAMIC
MONITORING
Current methods of BP Monitoring include:
The invasive method which is intra-arterial monitoring used in operating theatre and intensive care units. It involves piercing an artery with a cannula needle connected to a digital monitoring device.
There are also the non-invasive methods which include: a. The auscultatory method (also known as the Riva Rocci Korotkoff or manual method for blood pressure measurement) is the LISTENING of Korotkoff sounds in the brachial artery. The gold standard for clinical blood pressure measurement has always been to take a blood pressure using the auscultatory method where a trained healthcare provider uses a sphygmomanometer and listens for the Korotkoff sounds using a stethoscope. However, there are many variables that affect the accuracy of this method and numerous studies have shown that physicians and healthcare providers rarely follow the established guidelines for taking proper manual blood pressure measurements (Pickering et al, 2005). b. The oscillometric method is the measuring of the pressure variations in the blood pressure cuff caused by the oscillation of blood flow through the brachial artery. The blood pressure values are then calculated by an empirically derived algorithm. Most automated blood pressure monitors use the oscillometric method for blood pressure since is it less susceptible to external noise.
VII. BLOOD PRESSURE MEASUREMENTS
Blood pressure is always recorded as 2 numbers, such as 120/80, where the top number is the systolic pressure and the bottom number is the diastolic pressure. Systolic pressure is the pressure on the arteries as the heart contracts and pumps blood. The diastolic pressure is the pressure on the arteries when the heart is at rest in between heartbeats
VIII. ABOUT THE WEARABLE DEVICE
The wearable device will be designed like a wrist watch equipped with an inflatable wrist band and an optical bio sensor. A pump in the wrist band inflates to make sure the pressure is forced onto the wrist and that is how it takes the blood pressure. Blood pressure readings can also be taken through the biosensor that rests against the radial artery in the wrist, it detects the shape of the pressure wave as blood flows through it. A 128 gigabyte memory stores blood pressure measurement data daily which could be accessed from the watch’s application on an android phone. The wearable device will have a Nano sim connected to a network provider for dialing emergency numbers when blood pressure reaches a life-threatening level.
IX. HOW THE DEVICE WORKS
The watch takes reading at the press of a button. Automatic reading also gets done throughout the day and especially at night with the Biosensor. To get blood pressure reading the watch needs to be at the heart level. Watch vibrates 3x when blood pressure measurement is at risk and continuously when high and life threatening, when blood pressure gets to such a level, the watch sends an emergency call to numbers added to the emergency list which could be a family member, care giver or health worker.
The watch also will measure daily activity, heart rate, and sleep quality, and will be able to be set to read blood pressure while the user is sleeping (so long as they are wearing the watch)
The device will take blood pressure measurements from the radial artery which is 2.35 +-0.49 mm in diameter thinner than the brachial artery which is 3.97+-0.51mm thicker. The device is first calibrated with a standard blood pressure monitor. The device will work with a special algorithm whose indices can be processed to get heart rate, diastolic and systolic pressure, and other measures.
X. THE BIOSENSOR
Biosensor uses the characteristics of light in a very special way and it is called the optical power modulation (OPM). When the bloods flows through the arteries, there are several ways in which it causes movement within the tissues and it flows in straight line. There is also the pulse flow which is not linear in response to heart beating. The artery walls move in response to blood flows and the tissues surrounding the arties expand and constrict hence a micro motion occurs. This technology is a micro motion detector. There is a button that sits against the wrist and picks up the micro motion at the skin surface, and as the button moves backward and forwards it imparts a beam of light and as the light changes because it has gotten interference from this button the device is able to form the pattern of that light change provide the blood pressure readings that help to know what blood flow is like, and from the blood flow you can get the blood pressure reading.
XI. FACTORS TO ENSURE ACCURACY OF MEASUREMENT
This wrist monitor, if used properly, is quite effective, however the exact procedures and directions must be followed to get results that are accurate. The position of the body affects the accuracy of this monitor, so one need to be very careful when using it. Doctors say that the wrist and arm need to be at the level of the heart, to get an accurate reading. So, the following precautions are necessary for accuracy:
Proper Positioning: This is necessary for getting accurate readings is the positioning. Whether it is an upper arm or wrist, they should be at heart level.
Device should be worn on bare wrist not over the shirtsleeve
The device’s accuracy must be checked annually at the doctor’s office
The device must be fully charged before wearing and BP measurement as low battery charge may affect accuracy.
XII. BENEFITS OF AMBULATORY MONITORING USING THE WEARABLE BP MONITORING
Ambulatory BP monitoring provides additional information about how your changes in BP may correlate with your daily activities and sleep patterns. The United States Preventive Services Task Force (USPSTF) now recommends confirming a diagnosis of hypertension with ambulatory BP monitoring.
For most people systolic BP decreases about 10%-20% during sleep. However, for some people BP might not drop during sleep and may even rise.
Ambulatory BP monitoring can detect abnormal fluctuations in BP that might go unnoticed when BP is only measured in the doctor’s office. It is a very useful way to detect white coat hypertension, masked hypertension, and sustained hypertension:
• White coat hypertension: Some people who do not take BP lowering drugs (antihypertensive drugs) have elevated BP readings when their BP is taken at a doctor’s office or other health care setting. This is known as “white coat hypertension.” White coat hypertension can result in misdiagnosis of patients whose BP is actually normal. White coat hypertension has been observed in 15%-30% of patients with elevated BP readings. When ambulatory monitoring yields readings within the normal range outside the doctor’s office, patients usually do not need to take antihypertensive drugs.
• Masked hypertension: This condition occurs when a patient’s BP reading is normal at the doctor’s office but is elevated when the patient is at home. It may occur in up to 20% of people who are being treated for hypertension.
• Sustained hypertension: This refers to BP readings that are elevated whether the patient is in the doctor’s office or at home. This condition has been linked to an increased likelihood of heart and kidney damage.
Ambulatory monitoring can rule out white coat hypertension, so that patients are not given unnecessary prescriptions for BP-lowering drugs. It can also detect masked hypertension, so that patients receive the medications needed for high blood pressure. The incidence of stroke, heart disease, and organ damage due to hypertension can be reduced among those patients. Ambulatory monitoring may also be
useful in evaluating a patient’s response to long-acting antihypertensive medications.
The drug reminder on the wearable device will be very helpful in reminding the hypertensive patient of the time to take drugs.
Critical BP alert and emergency calling on this device will be very beneficial in saving those in danger of cardiac arrest.
CONCLUSION. Given the nature of high blood pressure and the population that is suffering from it in Nigeria and across the globe, it has become a matter of urgency to adopt a wearable device like the one discussed in this work to enable those who have this sickness manage themselves better to prolong their life span. Mobile health (mHealth) is becoming the order of the day, and health care is moving from hospitals to homes, so a wearable blood pressure monitor will be a move in the right direction.
ACKNOWLEDGMENT
This work was supported by Loyola Marymount University under the supervision of Professor Ma, Kuo-sheng, Professor of Biomedical Engineering for Fall Semester 2018.
REFERENCES
[1].https://www.wearabledeviceblog.com/how-smart-watches-measure-blood-pressure/
[2].https://myhealthdevices.com/are-wrist-blood-pressure-monitors-accurate
[3].http://www.bloodpressureuk.org/BloodPressureandyou/Thebasics/Bloodpressurechart
[4].https://healthtechinsider.com/2018/06/12/omron-to-debut-oscillometric-blood-pressure-watch/
[5].https://cdnsecakmi.kaltura.com/p/684682/sp/68468200/thumbnail/entry_id/1_q9g0r4dj/version/100012/width/718/height/431
This is good work to sustain human life and reduce untimely deaths due to ignorance and negligence. Congratulations and keep it up and ensure its realization.
Thanks Honourable. I have no funds to achieve the goal. I have provided a theoretical framework for its conceptualization. Someday, someone or some group will take up the idea and bring it to fruition.